HY-FOLIC®'S ROLE IN MAINTAINING HEARTH AND BLOOD VESSEL HEALTH
Cardiovascular disease is one of the most burdensome global public health challenges of the 21st century. Particularly in developing countries, the burden of cardiovascular disease continues to increase. Between 1990 and 2020, the number of people with coronary heart disease is estimated to have increased by 120% for women and 137% for men [1]. According to data from the 2023 National Health Survey (RISKESDAS), the prevalence of heart disease in Indonesia reached 30.8%.
Cardiovascular disease, also known as heart disease, refers to several diseases such as: coronary artery disease (CAD) or coronary heart disease, cerebrovascular disease, and peripheral artery disease. Coronary heart disease is caused by reduced myocardial perfusion, leading to angina (chest pain) and myocardial infarction. Cerebrovascular disease is associated with stroke and transient ischemic attacks (mini-strokes). One of the primary causes of these cardiovascular diseases is atherosclerosis, or the build-up of plaque in blood vessels.
Atherosclerosis and its Relationship to Cardiovascular Disease
Atherosclerosis is an inflammatory disease of the arteries and is the leading cause of cardiovascular disease (CVD) and stroke. In patients with atherosclerosis, the arteries narrow due to the accumulation of lipids and inflammation of the arteries, causing the arteries to harden and impairing blood flow, which can lead to the heart or brain being deprived of oxygen. If atherosclerosis is left untreated over the long term, it can lead to coronary artery disease (CAD), the most common form of cardiovascular disease (CVD), which can ultimately result in clinical complications such as myocardial infarction (MI) and stroke. As a disease with slow progression, clinically significant atherosclerosis primarily occurs in the elderly [2].
Lesions or atherosclerotic plaques can be caused by several factors, including:
The growth of this lesion will become more severe and can reduce blood flow by >50%, potentially causing a heart attack (angina) during physical activity/exercise or stress. The lesion may become unstable and rupture, causing a wound that triggers coronary artery blockage by blood clotting factors, potentially leading to a clot in that area and obstructing blood flow to the heart, which can result in myocardial infarction. The clot may also exit the heart and travel to the brain, potentially causing a stroke [2].
Stroke and Blood Vessels
A stroke is a condition in which a person experiences neurological deficits that are clinically caused by vascular injury (infarction or blockage and bleeding in the brain) to the central nervous system in the brain. Stroke is the second leading cause of death and disability worldwide. Stroke is not a single disease condition but is caused by various risk factors and complications from other underlying conditions, such as diabetes, hypertension, and coronary heart disease.
Strokes can be classified as ischemic strokes or hemorrhagic strokes. Ischemic strokes are caused by a lack of or loss of blood supply to an area of the brain and are the most common type of stroke. Hemorrhagic strokes are caused by bleeding in the brain due to a ruptured blood vessel.
Most (about 85%) strokes are caused by blockages in the blood vessels in the brain, which result in a lack of oxygen supply to the brain, commonly known as ischemic stroke. Ischemic stroke is usually caused by atherosclerosis in the small blood vessels in the brain, cardioembolism, and atherothromboembolism in the large arteries in the brain.
Post-stroke patients are prone to other complications, especially those arising from the brain injury itself, such as disability or immobility, cognitive impairment, and neurological disorders.
Homocysteine, Hyperhomocysteine, and Cardiovascular Disease
Homocysteine is an amino acid formed from the metabolism of methionine. 5-MTHF is the active form of folate involved in the remethylation of homocysteine to methionine, a process that is very important for maintaining normal homocysteine levels in the body. In addition, this process also plays a role in the expression of DNA formation genes in methylation reactions. Methionine metabolism occurs through one-carbon metabolism, which requires 5-MTHF (active folate), vitamin B6, and B12. However, the balance of this metabolism can be disrupted due to a deficiency of 5-MTHF (active folate).
Folic acid deficiency can occur due to insufficient intake of folic acid from food sources or supplements and genetic mutations in the MTHFR polymorphism. Disruption of homocysteine metabolism can lead to the accumulation of homocysteine in the blood (hyperhomocysteinemia) [11]. Cross-sectional studies examining homocysteine, vitamin B, and stroke indicate that vitamin B levels should be increased and homocysteine levels reduced to prevent stroke [12].
Hyperhomocysteinemia is a condition in which homocysteine levels in the blood are outside the normal range of 5–15 mmol/L. Hyperhomocysteinemia is categorized into three stages: mild (15–30 mmol/L), moderate (30–100 mmol/L), and severe (>100 mmol/L).
Hyperhomocysteine can cause various health problems. If left untreated, this condition can trigger heart diseases such as atherosclerosis and stroke. This occurs because homocysteine is toxic to blood vessel endothelium, increases LDL oxidation, and triggers blood clot formation [3].
Endothelial cells in blood vessels act as regulators of blood circulation homeostasis and blood vessel walls, functioning like gatekeepers of heart health. Endothelial cells play a crucial role in regulating blood vessel wall homeostasis, including vascular tone, coagulation, inflammation, and permeability. As cells directly exposed to blood, endothelial cells are susceptible to damage from various risk factors that can lead to endothelial dysfunction and endothelial barrier damage. This damage can trigger a series of domino effects on heart health, such as inflammatory responses, monocyte recruitment, plaque formation, structural changes in the heart, and thrombosis (blood clot formation).
Based on studies, it indicates that hyperhomocysteinemia can damage endothelial cells and cause endothelial dysfunction. Several other studies confirm that homocysteine concentration is associated with atherosclerosis. Clinical studies show that plasma Hcy levels in patients with coronary artery disease are significantly higher than in control groups with normal angiography results. Even elevated plasma Hcy levels, even if only 12% above the upper normal limit, have been associated with a 3.4-fold increase in the risk of myocardial infarction (heart attack) [3].
A study published in the Journal of the American College of Cardiology (JACC) in 2024 found that homocysteine levels (tHcy) are positively associated with myocardial injury and cardiovascular mortality, further strengthening the link between HHcy and CVD events [4].
Another study by the International Renal Research Institute in Italy in 2017 found that 85% of patients with chronic kidney disease had hyperhomocysteinemia [5]. This reinforces the association between hyperhomocysteinemia and an increased risk of cardiovascular disease and kidney damage.
Folate Deficiency Causes Hyperhomocysteinemia
Folate deficiency can lead to elevated homocysteine levels in the blood, which is associated with an increased risk of cardiovascular disease and kidney damage.
Clinical Evidence of the Benefits of Folate for Cardiovascular Health
Folate supplementation has been shown to be beneficial in reducing the risk of stroke (prevention) and managing blood pressure through the reduction of hyperhomocysteinemia.
A clinical study by Mazza, A., et al. in 2016 showed that administration of 5-MTHF (Active Folate) 400 mcg can reduce homocysteine levels by up to 55.8% compared to baseline conditions [6].
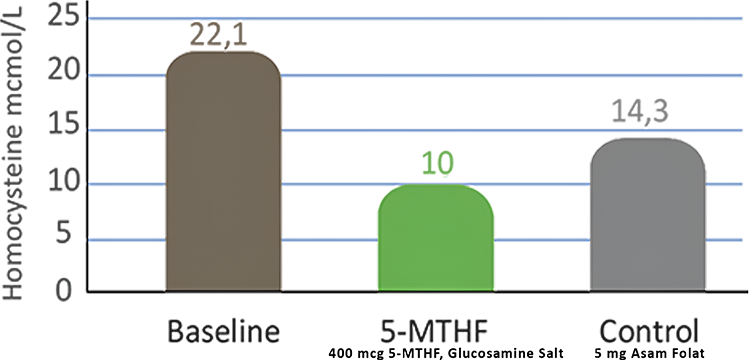
Image. Comparison of the effectiveness of 5-MTHF (Active Folate)
in reducing homocysteine compared to folic acid.
Another large-scale study in China, involving more than 20,000 hypertensive patients, showed that the use of folate in patients receiving antihypertensive therapy can significantly reduce the incidence of stroke and progressively reduce the risk of kidney function [7].
Evidence Based
The study by Huo, et. al. (2015), showed that folate administration in patients receiving antihypertensive therapy (n=10,348) can reduce the incidence:

The study by Xu, et. al. (2016), showed that folate administration in patients receiving antihypertensive therapy can reduce the incidence:
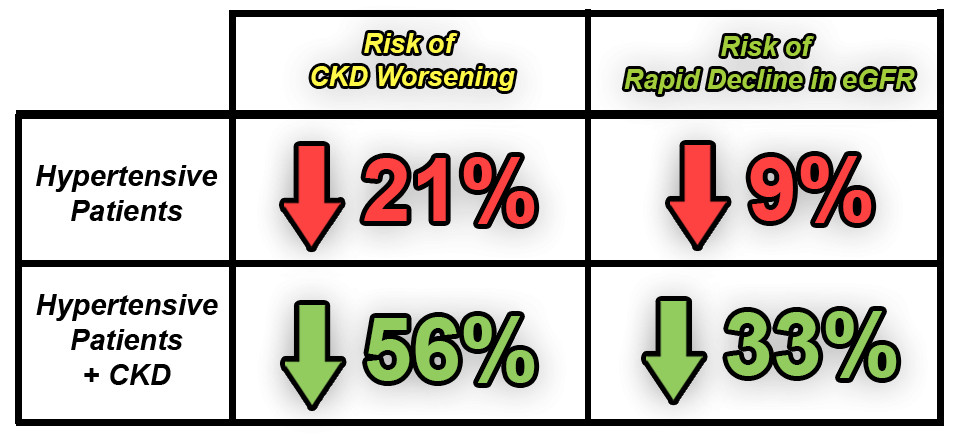
Supplementation of 5-MTHF (Active Folate) Can Improve Heart Health
Supplementation of 5-MTHF (Active Folate) can improve heart health and prevent the worsening of chronic kidney disease by lowering hyperhomocysteine levels.
Conclusion
HY-FOLIC® plays a crucial role in maintaining heart and blood vessel health through its ability to optimize homocysteine metabolism. As the active form of folate, 5-MTHF in HY-FOLIC® helps convert harmful homocysteine into methionine, thereby preventing the accumulation of high homocysteine levels or hyperhomocysteinemia. Given that hyperhomocysteinemia is a major risk factor for atherosclerosis, endothelial damage, increased LDL oxidation, and blood clot formation—which can lead to coronary heart disease and stroke—supplementation with HY-FOLIC® is an important strategy for mitigating these risks.
Solid clinical evidence shows that folate supplementation, such as HY-FOLIC® that contains 5-MTHF (Active Folate), can significantly reduce the incidence of stroke and the risk of worsening kidney function, confirming its role in the prevention and management of cardiovascular disease. Therefore, HY-FOLIC® can be an effective solution in maintaining overall heart and blood vessel health.
References: